From three-dimensional (3D) pre-surgical simulations to augmented reality (AR) guidance during an operation - coming soon - technology has cut its way into the surgical ward.
The result: Better patient outcomes.
According to Dr. Solomon Dadia, surgical innovation is a “multifaceted” term. As the head of the Levin Center of Surgical Innovation and 3D Printing Unit and deputy director of the Orthopedic Oncology Department at Tel Aviv Sourasky Medical Center, Dadia has spent the last six years collaborating on innovative approaches to improving surgical processes and outcomes. He has also served as a matchmaker between technology companies looking to integrate into the clinical world and surgeons who have medical ideas and needs that through technology could be made a reality.
The center is composed of doctors, engineers, product designers and radiology experts, who meet together to come up with the next big clinical innovation.
One area already in practice is the use of 3D printing. By using computer software, layers of two-dimensional diagnostic images from CT and MRI can be converted into 3D images that are then printed and provide “one very beautiful” physical rendering of the organ or body part at hand.
“It is amazing,” Dadia told The Jerusalem Post. “I don’t think our mind can even process all those images together.”
Before 3D printing, variant scans were delivered to surgeons in 2D pictures, and the doctors were forced to scroll up and down and create a 3D image in their minds. Now, “when all the data is in one image,” Dadia explained, “the doctor can better understand the pathology and anatomy, plan and design the surgery and tackle any potential problems before they happen.”
The technology is particularly important in Dadia’s field of orthopedic oncology, where surgeons are repeatedly called upon to excise malignant bone tumors without destroying the bone. If any of the tumor is left behind, the individual could relapse.
This is especially important when it comes to children, whose bones are still growing, or in cases where a tumor needs to be removed near a joint. By printing a 3D model in advance of the surgery, the location of the tumor and its exact boundaries can be assessed and the removal of it done with utmost precision, improving the patient’s life, Dadia explained.
“We can print the models on multi-color, multisensory materials that can mimic human tissue and the surgeon can do a dry run before the operation,” he said. “This is happening every week in our innovation center.”
The team is also providing 3D-printed casts for upper limbs.
Dadia said that individuals who come to the ER with a broken arm can have their limb scanned with a 3D scanner and then a cast created within only a couple of hours. Unlike traditional casts, which are heavy, dirty and that must be kept away from water, these are light, comfortable and aesthetic and “you can go swimming the next day,” Dadia said.
Moreover, because the cast is made specifically for the individual’s broken limb, it is less likely to have unintended pressure points, which can cause chafing and bruises.
Sourasky is the only hospital in Israel currently providing the casts; they are not yet available for lower limbs and are not covered by insurance, so cost close to NIS 1,000.
Up Next: 3D-printed organs and augmented reality
Moreover, the lab can print patient-specific instruments for use during the surgeries, Dadia said. They are printed from biocompatible materials that have been validated by the Food and Drug Administration.
And, it is now working on producing bone and other implants, as well.
Today, bone implants are generally made of plastics, titanium or other metals that can cause infection, mechanical loosening and lead to repeat surgeries. Dadia said his lab is working with teams in Israel and Europe to develop hybrid implants with 3D-printed biological filler that Dadia believes could be available even within the next two years.
“There will be prints made of bio-ceramic, biodegradable materials, which we can implant in children, so that the bone grows and the foreign material dissolves as the child grows,” Dadia said.
And he envisions that from there, the transplantation of 3D-printed organs into human bodies will come.
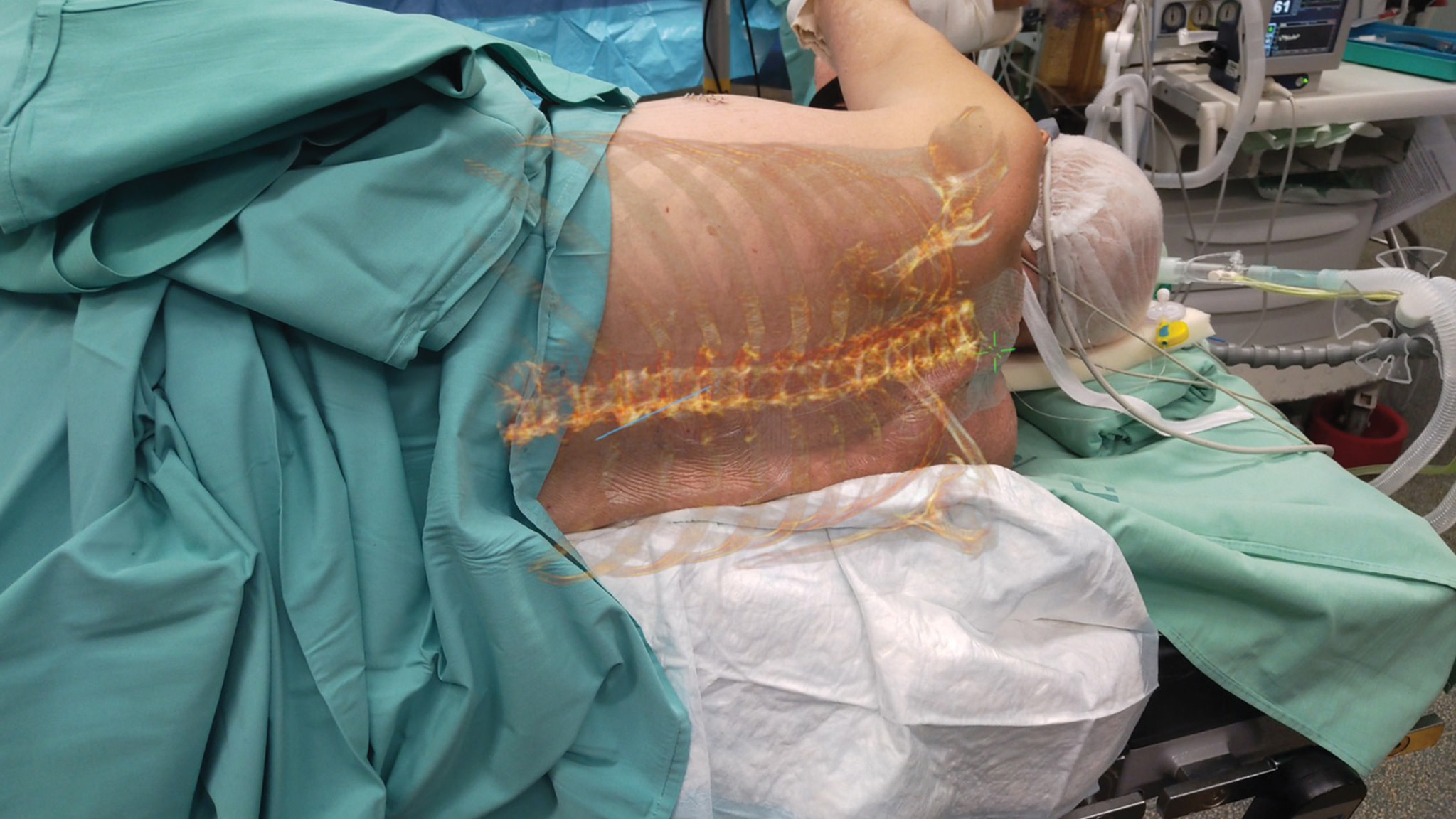
Finally, Dadia said that augmented reality glasses are already being used in some instances at Sourasky and he believes that within the next two years, the full blown technology with all its aspects of patient registration and guidance will be ready and implementable.
Dadia said that surgeons tend to be conservative and the medical field in general often struggles to keep pace with technology. However, he believes that the more innovation can be integrated into the clinic, the better the surgical workflow will be, the more exact procedures will take place and that patient results will improve.
“This could be anything from a robot to a new tool or software,” he said. “I find that in the operating room there are huge gaps in technology. We are trying to close those gaps.”
Today, the innovation center is working with around 40 companies - companies that at the beginning his team was chasing after, but now “they come to us.”
“The collaboration with the industry is the heart of all this activity,” he said.
Next, Dadia is hoping to get some of the newest innovations covered by the Health Basket. He said he is working with the Health Ministry to achieve that goal.
“Hopefully by the end of 2022 the ministry will embrace this technology nationally. If that happens, it will really open the doors.”
This article is taken from The Jerusalem Post Israel Technology and Innovation Magazine 2022. To read the entire magazine, click here.
This article was written in cooperation with Levin Center