Machine learning – the application of artificial intelligence (AI) using computers – can be utilized to match a cancer patient with the best immunotherapy.
This process – using mathematical models of data to help a computer learn without direct instruction and continue learning and improving on its own based on experience – can now help oncologists decide what specific treatment should be used.
Cancer specialists are not the only ones who want to know this, but also health maintenance organizations and private health insurance companies. This is because immunotherapy or biotherapy – which helps the immune system fight cancer using white blood cells, organs and tissues of the lymph system – is very expensive.
The study
Now, a new study by Prof. Keren Yizhak of the Rappaport Faculty of Medicine at Haifa’s Technion-Israel Institute of Technology uses AI to create a simple and inexpensive method of answering this question for each individual patient.
Her findings were recently published under the title “Estimating tumor mutational burden from RNA-sequencing without a matched-normal sample” in the prestigious journal Nature Communications and selected to be featured in the “Editor’s Highlights” webpage on cancer.
The study was led by Dr. Rotem Katzir and bachelor of science student Noam Rudberg, both from the Taub Faculty of Computer Science.
Background to the study

Immunotherapy is a recent development in the world of cancer treatments and has put patients who could not be helped by other means into full remission. It also reduces many of the side effects of chemotherapy.
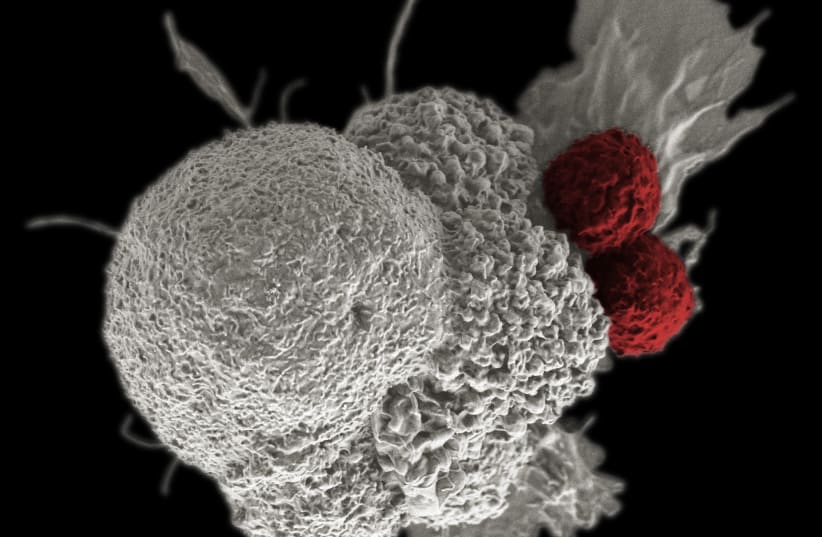
There are numerous immunotherapeutic treatments, but they differ from the new study since the principle under which they all operate is stimulating the patient’s immune system to attack the tumor cells.
How does the immune system distinguish between the cancer cells it should attack and the healthy cells of the body? The more mutations the tumor has accumulated, the more it differs from the “normal” cells, and thus immunotherapy can be more effective. This characteristic is called tumor mutation burden. A higher TMB means more new mutations. Yitzhak’s method significantly simplifies measuring it.
TMB is currently measured by taking cells from the tumor and comparing their DNA to that of the patient’s healthy cells. Yizhak and her team suggest making two changes in this process.
The first change, already explored in a previously published article by the group, is comparing RNA molecules rather than DNA ones. This makes a difference because DNA molecules contain the entirety of the human genome while RNA ones are small parts of the genetic code that are copied out to be used as instructions within the cell. In their previous study, the group showed that RNA molecules can also be used to identify cancer-specific mutations.
What does it all mean?
Their discovery is significant because it eliminates the need to compare the RNA from the tumor to DNA from healthy cells.
As a result, a smaller amount of genetic material needs to be sequenced, allowing the patient to be subjected to one less procedure. Instead of comparing the genetic material from the tumor to the patient’s own healthy genetic material, they developed a machine-learning algorithm that was trained to recognize aberrations from the healthy genome and to tell them apart from the natural variation that exists between people.
Second, using these predictions, they were able to compute an RNA-based TMB metric. In fact, this method proved to be more effective than the standard method in estimating the predicted effectiveness of immunotherapy for a given patient. This is thought to be the case because the RNA contains the parts of the genome that are in constant use and can therefore initiate an immune response. Mutations in parts of the genome that are not in use are less likely to affect the cell’s operation.
The development of the algorithm was made possible by using a large existing database on which the computer could be trained regarding sequenced RNA from cancer patients. Yizhak’s laboratory is actually a computational “dry” lab – rather than one with test tubes and other paraphernalia to experiment with real substances – that makes use of the large amounts of clinical data collected by the scientific community around the world to make new discoveries and develop new tools to assist patients.